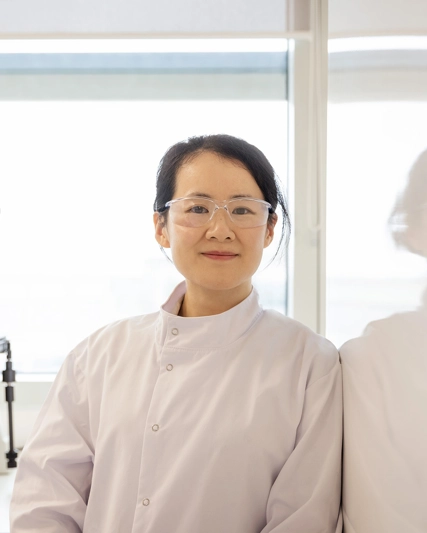
Dr Tony Wood
Chief Scientific Officer

Tony Wood, GSK’s Chief Scientific Officer since 2022, leads all Research and Development activities across GSK’s portfolio and pipeline, with a specific focus on driving delivery of new, innovative medicines and vaccines that bring transformative impact for patients in areas of high unmet need. He leads a global organisation focused across four core therapeutic areas (respiratory/immunology/inflammation, oncology, HIV and infectious diseases) and driven by three R&D priorities – Execution, Technology and Culture – all central to developing an R&D approach based on the science of the immune system, human genetics and advanced technologies, notably building ground-breaking in-house capabilities in functional genomics, artificial intelligence and machine learning, as well as through focused business development and partnering.
Tony is one of the world’s pre-eminent medicinal chemists and has the rare distinction of inventing one of the first mammalian host protein-targeted anti-HIV drugs to reach the market. As a pioneer of structure-based drug design to overcome problems of resistance, he has striven to advance strategies in medicinal chemistry design, including ligand efficiency and lipophilic efficiency, structural-property relationships for toxicity, and the use of chemoinformatics to inform molecule and library design.
He is a Fellow of the Royal Society, a Fellow of the Academy of Medical Sciences and a Fellow of the Royal Society of Chemistry. Tony has a BSc in chemistry and a PhD in organic synthesis from Newcastle University.
There’s never been a time when science and technology have formed such a powerful union as they do now. We’re able to identify drug targets using genomics and AI/ML in a way that is unprecedented. We are also able to use more approaches than ever before to design new vaccines and medicines to address the root cause of disease.