How can someone tell if they have a common cold, or a more serious virus like RSV, flu or COVID-19? According to respiratory and population health experts, the answers lie in the sometimes subtle but unique symptoms each infection causes – and being able to tell the difference could be lifesaving.
The ‘common cold’ is the most frequently caught infection worldwide. According to the American Lung Association, most adults can expect to get between two and four colds every year.
There are more than 200 different viruses that can cause colds. However, they rarely have serious consequences and people tend to get better on their own.
The trouble is the symptoms of the common cold can be similar to other, potentially more serious respiratory infections that may require hospital treatment. This category of infections includes influenza, or flu, respiratory syncytial virus, or RSV and COVID-19.
Flu is estimated to affect up to one in five of the population each year, leading to between 100,000 and 710,000 hospitalisations in the US annually.
And although case numbers for COVID-19 globally have dropped since the height of the pandemic, it is still causing thousands of hospitalisations.
Meanwhile, RSV is estimated to affect more than 5 million people over the age of 60 in higher income countries in North America, Europe and South-East Asia. Most people recover easily, but those with underlying health conditions, such as diabetes, COPD, asthma, coronary artery disease or heart failure, are more at risk for severe illness.
RSV causes up to 470,000 hospitalisations and up to 33,000 in-hospital deaths among this age group in affected nations every year. Despite this, only 6 in 10 adults over the age of 50 have ever heard of RSV, according to a 2024 GSK survey. Concerningly, a 2025 study by GSK showed that adults aged 50 and over with certain chronic underlying health conditions underestimate their personal risk of severe RSV illness despite a higher chance of serious illness and hospitalisation compared to people without these conditions.
Timing and severity
Early signs and symptoms can help with the identification of a respiratory infection and indicate whether someone needs additional support from a healthcare professional.
"When it comes to respiratory infections, the timing of symptoms can be a key indicator of their severity," says Professor Alberto Papi, Chair of Respiratory Medicine at the University of Ferrara.
Symptoms of the flu, for example, tend to come on quickly, while RSV can take 4-6 days after infection before it becomes obvious. COVID-19 may show no or only mild symptoms for a few days after infection, only to escalate later.
While not everyone with flu experiences a fever, it is a more common feature of the virus than for those with COVID-19, who are more likely to experience mild body aches and chills. Loss of smell or taste became a common symptom of COVID-19 in earlier cases of the infection. However, the same symptoms can be experienced with the flu, RSV, and sometimes with the common cold, the latter usually owing to congestion.
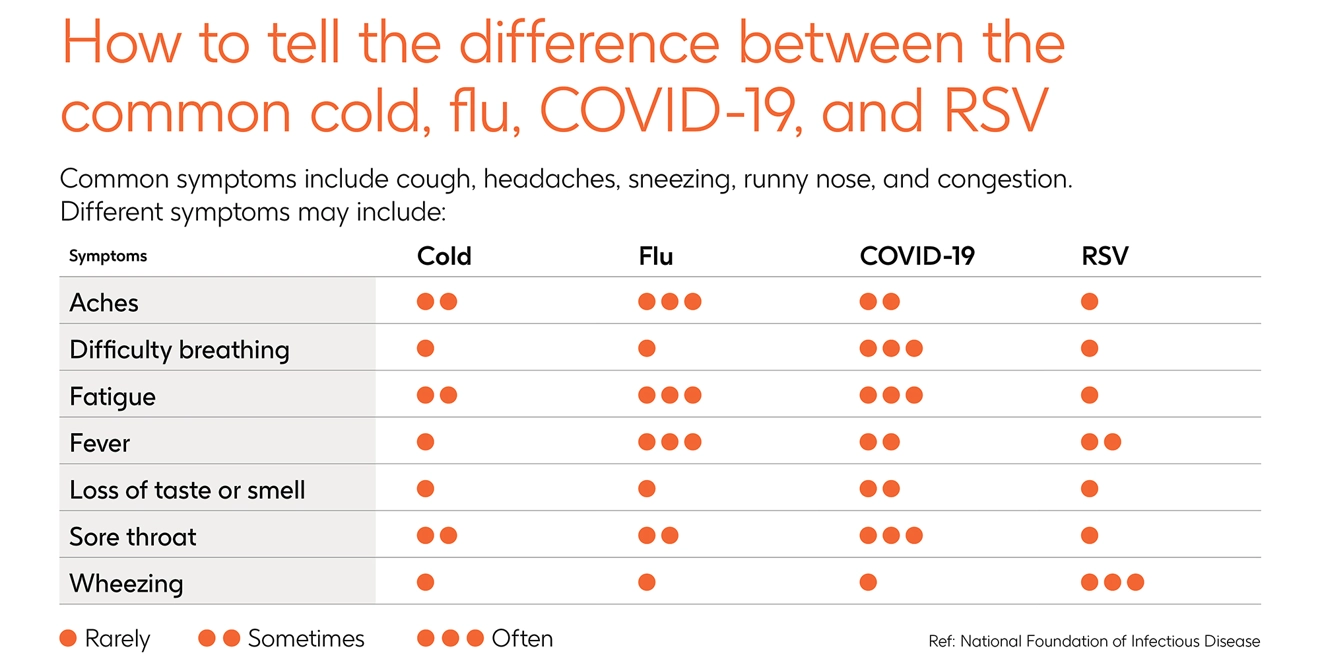
Take a look at our symptoms checker for a simple overview of the indicators of some symptoms in different infections:
Of course, these respiratory infections are experienced differently by individuals, making it difficult to predict infections based on symptoms alone. People should seek an over-the-counter test where available, or via a healthcare professional as soon as possible. Waiting or self-treating can lead to complications, especially in vulnerable populations such as those with underlying medical conditions, older people or infants.
"While it's true that the symptoms of RSV, COVID-19, and seasonal flu can be very similar in the initial phase, we now have appropriate tools to establish the right diagnosis irrespective of those initial symptoms,” Professor Papi continues.
“Early intervention by seeking medical help not only can save lives but also prevent the progression of the disease, especially in high-risk populations.
“Recognising signs early and acting swiftly is paramount."
The type of infection
The type of respiratory infection someone may be at risk from depends on the viruses circulating around a general population at any given time. Each year many countries conduct surveillance for viruses including RSV, COVID-19 and seasonal flu. These reports provide a warning for front line health professionals and health systems of possible surges in cases and potential epidemics.
“Factors such as levels of immunity in the community and the precautions we take against respiratory infections can influence its impact,” says Frithjof Kosfeld, Medical Affairs Specialist at GSK.
However, RSV is very different from seasonal viruses like the flu, which has higher variability, meaning it mutates into different strains more frequently.
Strains of RSV that regularly cause human disease – which have only one viral type and two subtypes – do not have the same variability. This means that scientists are not chasing a rapidly moving target, as is the case with flu.
“Our knowledge of RSV continues to grow, and we are committed to gaining a deeper understanding of the behaviour of RSV particularly its risk to people with certain underlying conditions,” Kosfeld adds.
“By increasing our understanding, we have made significant progress in preventing severe outcomes in higher-risk populations. As I’ve learned from great patient advocates, with knowledge comes empowerment – for people to make the right decisions about their health.”
Preventing infection
Recommended practices aimed at reducing the spread of respiratory infections include maintaining good hygiene and reducing social contact with others when infected, as well as wearing a mask in public indoor and crowded spaces.
Routine vaccinations also protect individuals against infection and importantly can reduce the severity of symptoms when someone does become infected.
“In the battle against infectious diseases, vaccinations have been nothing short of transformative, helping save millions of lives each year," explains Susie Barnes, SVP, Global Medical Affairs, Vaccines at GSK.
"However, the risk from these diseases is ever evolving, and our fight against them must adapt in kind. Continued research is crucial not only for improving existing vaccines but also for developing new solutions that can address emerging health threats."
This article was originally published in December 2024 and has since been updated.





