Asthma attacks and COPD exacerbations are frightening for patients, but the irreversible damage that occurs inside the lungs during even a mild attack makes preventing them even more important. Thankfully, scientists have a greater understanding of respiratory diseases than ever before, and preventative treatments are evolving which aim to improve health outcomes for patients.
Asthma and chronic obstructive pulmonary disorder (COPD) are different, but they progress in similar ways. Both are respiratory diseases, and both are chronic inflammatory conditions, driven by genetic and environmental factors.
Lung damage can occur when inflammation and exacerbations – or ‘attacks’– are not prevented. In just one attack, irreversible changes to the tissue of the lungs can occur, effectively leaving them scarred.
The damage may not cause problems initially, but with each attack or bout of inflammation, the tissue scarring gets cumulatively worse, eventually causing a permanent loss of lung function. This means a patient’s ability to breathe properly becomes increasingly difficult, and not enough oxygen is delivered throughout the body. As a result, the patient’s overall health suffers, which could prevent them from living the high quality of life they deserve.
But there is new hope on the horizon.
Scientists – including those at GSK – now know more than ever about the causes of respiratory diseases. This has led to new treatment paths and more ambitious treatment goals – including achieving clinical remission for some patients with severe asthma.
“What also concerns me as a physician is what is happening inside the lungs, the cumulative lung damage, the progressive changes to lungs even with what may be considered a mild attacks,” says Professor Ian Pavord, a leading respiratory expert at the University of Oxford, UK.
“Medicine has evolved and there is so much we can do to prevent the exacerbations and the irreversible lung damage.”
Biological pathways
Growing scientific knowledge of the biological pathways that influence asthma or COPD has helped healthcare professionals move away from a ‘one-size-fits-all’ treatment model to a patient-centred approach. This has been an important step forward because they now know that asthma and COPD are experienced differently by people.
One way scientists can identify these differences is by using biomarker testing. Biomarkers are characteristics of the body or disease – such as genes, proteins, or other substances – that can be measured to provide information about a patient’s biological condition or specific disease.
Once the unique characteristics of the patient’s disease have been identified through testing, doctors can gain new insights, including what treatments to suggest, as some treatments may only work for people who have certain biomarkers.
For example, a specific biomarker can be identified by analysing a simple blood test to work out which type of inflammation drives a patient’s asthma or COPD.
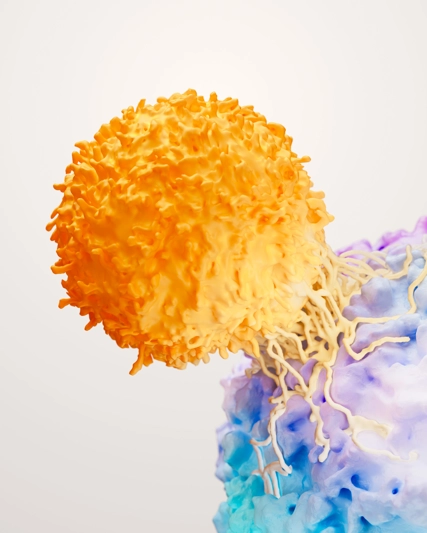
In more than 80% of patients with severe asthma, symptoms and exacerbations are driven by type 2 inflammation. Patients with type-2 inflammation exhibit elevated levels of eosinophils – a type of white blood cell.
By identifying elevated levels of these white blood cells via the blood test, doctors can speed up the diagnostic process.
“Medical advances, like the ones we've been able to make at GSK, means it is becoming possible to increase the understanding of the underlying causes of even the most severe cases of asthma and COPD,” says David Lipson, Vice President and Clinical Research Head, Respiratory at GSK.
“For people with asthma or COPD, we want to prevent their disease from progressing, and protect their lungs from damage.
“This damage can be avoided or minimised or, in the very least, we can prevent further damage. Patients can breathe easier today.”
Precision treatments
Over the last decade, biologic therapies have become increasingly available for patients with certain types of severe asthma, as well as other immune conditions.
Biologic therapies work by targeting specific bodily functions that cause symptoms like inflammation and asthma attacks. Unlike medicines that are made through chemical processes, biologics are made from living material such as proteins and sugars, substances already used as tools to carry out healthy biological functions in the body. As such, they can be designed to block the precise part of the immune system that is not working as it should while seeking to minimise the likelihood of affecting any healthy tissues or functions around it.
Despite the availability of biologic therapies, and the evidence that they can work, the treatments are underutilised. According to the Global Initiative for Asthma, or GINA, over 60% of eligible patients are not receiving these treatments. Many undergo multiple, potentially damaging, asthma attacks before they are given biologic treatments, too.
GINA also states that ensuring asthma and COPD patients are vaccinated against common respiratory diseases is also crucial, as they are more likely to develop severe complications from infections.
“People with asthma or COPD have often lived with their conditions for years, so their symptoms have become part of ‘normal life’,” says Tonya Winders, the President and CEO of patient advocacy organisation the Global Allergy and Airways Patient Platform (GAAPP).
“Few are aware that there are many more treatment options available to them now and that it may be possible to be free from symptoms and exacerbations. It’s time for this to change for the better.”
Greater protection
Preventing asthma and COPD attacks and minimising inflammation can prevent ongoing, cumulative lung damage, but what about the direct or indirect risk of damage to the rest of the body?
While highly effective in managing the symptoms of asthma and COPD, both frequent short and routine courses of oral corticosteroids (OCS) can cause numerous side effects and ultimately impact healthy parts of the body.
Short term effects of use include insomnia, indigestion, fluid retention and mood changes, while longer-term complications could involve osteoporosis, hypertension, cardiovascular disease, diabetes, increased risk of other infections and more.
Now, there is increasing evidence that the adverse consequences of OCS accumulate over a patient’s lifetime, even if they are receiving relatively low doses. Despite this and the availability of various biologic therapies which have shown to reduce the need for OCS, repeated courses of OCS are still frequently used as maintenance treatments, or ‘bursts’ and often prescribed before the underlying cause of a patient’s exacerbations or symptoms are understood. This approach may temporarily improve symptoms but does not address the specific underlying driver of inflammation in the long-term.
GINA recommends that OCS should only be considered as a temporary option. Meanwhile, GOLD 2024 – an evidence-based report that provides a global strategy for the diagnosis, management, and prevention of COPD – states that OCS should only be use during significant attacks, as even short bursts of treatment can increase the risk of pneumonia, sepsis, and even death.
“While OCS may be extremely effective in an acute setting to tackle inflammation and a ‘go-to’ for treatment of attacks, they can lead to complications further down the line,” says Prof Pavord.
“Yes, attacks must be treated to prevent lung damage as soon as possible, but it is also important that we predict and prevent attacks by assessing biomarkers and offering targeted preventative treatment.
“This way OCS will be used more sparingly, minimising the trade-off between lung damage from the asthma or damage to other organs from OCS.”
By addressing the root causes of asthma and matching the latest evidence-based treatments to the right patients, it could be possible for them to achieve clinical remission –stable lung function, and a life free from attacks, OCS, and symptoms caused by inflammation.
“I want people to know that they’re not causing a fuss by asking their doctor if being free from symptoms, exacerbations or the need for oral steroids could be possible,” GAAPP President Winders concludes.
“With today’s advances in respiratory medicine, we can all aim much higher.”