Cancer is one of the world’s biggest killers, but deeper understanding of individual cancer biology and an ever-increasing number of treatment options means patients could be more likely to make full recoveries in the future.
One of humanity’s biggest foes, cancer is second only to heart disease as a leading cause of death globally. Despite decades of progress toward improving survival rates for many common malignancies, diagnoses of certain cancers continue to increase. And although great strides have been made against some cancer types, many patients still have few treatment options available to them.
However, advances in technology and drug development across the industry have shown there is plenty of reason for hope.
Scientific understanding of cancer has accelerated in recent years, laying the foundations for a paradigm shift in the way the disease is diagnosed and treated.
For example, advances in artificial intelligence (AI) and machine learning are uncovering new leads across disease, including in oncology.
An explosion in genetic and genomic data is revealing novel ways of attacking cancer cells. New cancer therapies may promise greater effectiveness, and fewer side effects, than their predecessors. And an expanding menu of drug types means that doctors can use different tactics and combinations to treat cancer, potentially increasing the chances of patients making full recoveries.
These breakthroughs are taking place across industry and academia, and companies like GSK are partnering with academic researchers and advanced technology platforms to speed up research. GSK’s current focus is on haematologic malignancies, gynaecologic cancers and adjacent opportunities where a transformational outcome for patients is possible.
Chris Sheldon, GSK’s head of business development, says the combination of unmet need and scientific breakthrough has made cancer a key area where partnerships could have a real impact for patients.
“The world is a big place, and there’s just as much innovation happening outside our own four walls than in,” he says.
“By partnering with others, we’re able to achieve far more together than we could going it alone.”
Precision medicine
Not all cancers are the same. Some have characteristics, called biomarkers, that make them more likely to respond to certain treatments. Biomarkers are characteristics of the body or disease that can be measured to provide information about a patient’s biological condition or specific disease. They can include genes, proteins, or other substances.
Identifying these biomarkers, typically by testing biopsied tumour tissue or other biological samples like blood or urine, sheds light on the characteristics of the tumour and can indicate which treatments are likely to be most effective for patients.
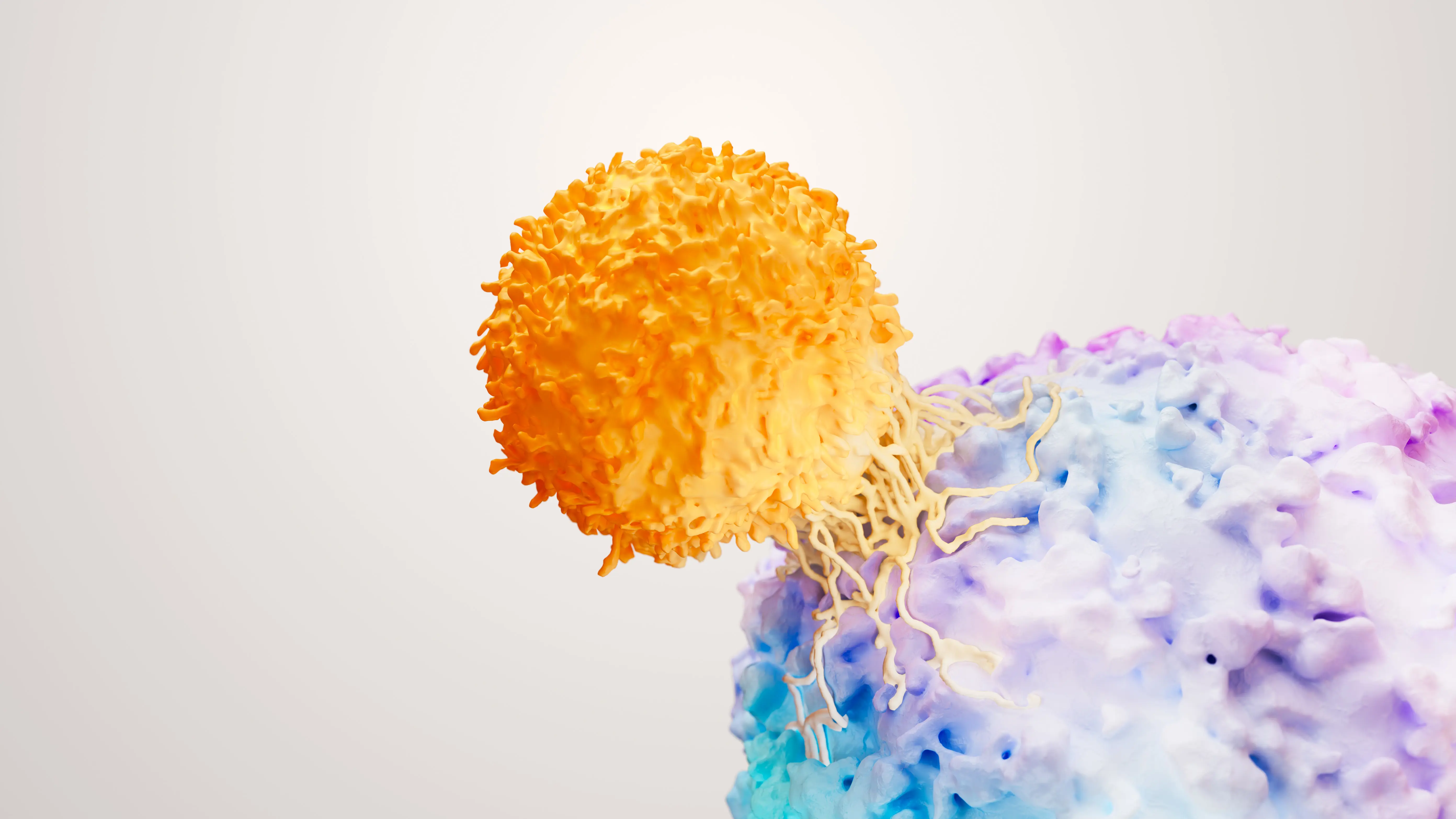
Some cancers have characteristics that could make them more susceptible to immunotherapies – therapies that help a patient’s own immune system recognise and attack cancer cells. They can be identified by a biomarker that shows that the cancer cell is unable to fix errors in its genetic code. Cancer cells that have this flaw are much more vulnerable to immuno-therapies than those that don’t.
One such biomarker, known as microsatellite instability, is found in 15-to-30% of patients with colorectal, stomach and endometrial cancers and at smaller levels in several other cancer types.
“We’re really trying to use genomics and biomarkers to match patients to appropriate precision therapies,” says Hesham Abdullah, Senior Vice President, Global Head of Oncology, R&D, at GSK.
“This aims to create a treatment effect for patients across both advanced and earlier stages of the disease.”
Targeted therapy
A major challenge in oncology is finding ways to kill tumour cells without also harming healthy cells or tissue. Chemotherapy is a powerful tool in fighting cancer, though while it is an effective killer of tumour cells, there can be a lot of collateral damage.
An important avenue of cancer research is developing drugs that can more precisely target malignant cells, sparing healthy tissue. Many of these new drug types are based on antibodies, molecules with intricate three-dimensional shapes that can be designed to complement structures on or near tumour cells like a lock and key. These antibody-drug conjugates (known as ADCs) gain access to the inside of tumour cells through this mechanism, where they deliver the intended drug.
“Having a broad range of treatment approaches is important because tumour cells can develop resistance to one treatment type,” Abdullah continues.
“Cancer cells are extremely smart, and they tend to develop these resistance mechanisms if you come at them with one mechanism.
“What we need is not only one mechanism, but combinations that come at it from two or more different angles.”
AI and machine learning
Many biomedical breakthroughs begin with pattern recognition. In the late 18th century, Edward Jenner’s observation that milkmaids who had fallen ill with cowpox were protected from smallpox led him to develop the world’s first vaccine.
More than two centuries later, an explosion of data and advances in analytic tools are vastly expanding the potential for pattern recognition – and medical breakthroughs across multiple disease areas, including in oncology.
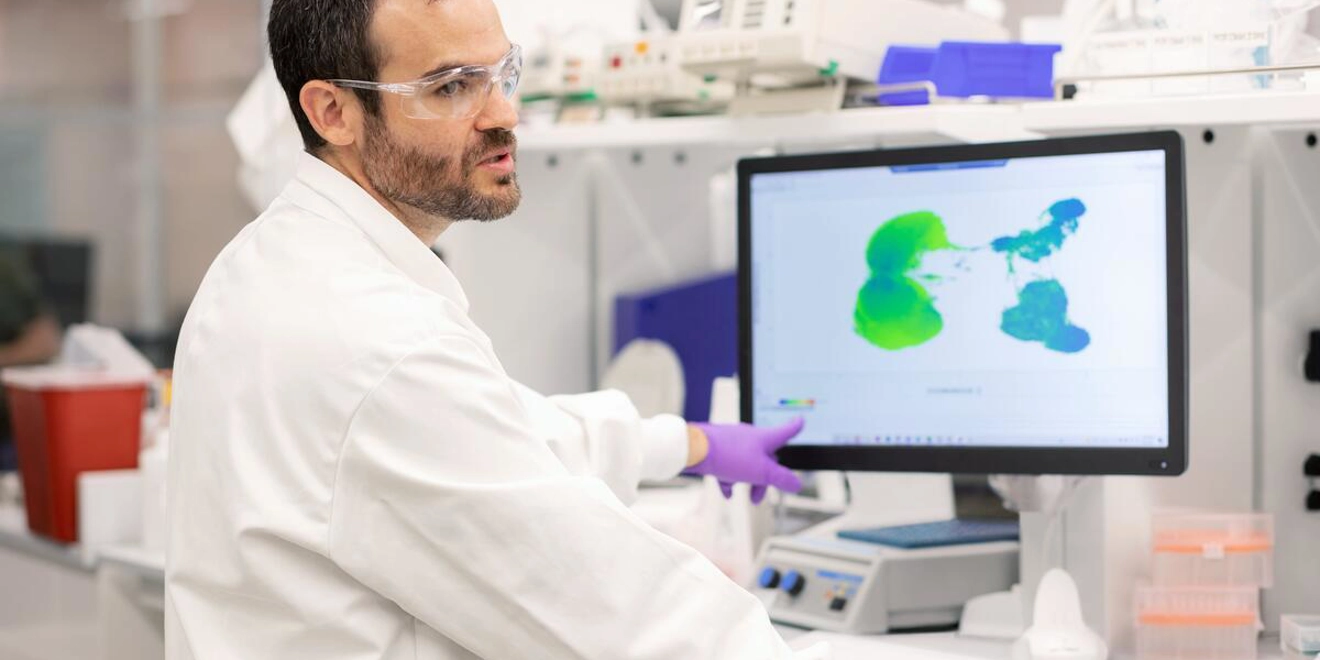
Genetic data, microscope images of tumour cells and diagnostic images from CT and MRI scans are just a few of the sources producing a wealth of new information to mine for patterns. AI and machine learning are making it possible to sift through vast and varied datasets at speed to discover meaningful new insights.
Advanced technology is being integrated into every stage of drug development, from selecting which molecules to take forward into early testing, to identifying the patient groups most likely to benefit from a drug.
“Every decision that you're making is predicated by data,” says Abdullah.
“At the end of the day, AI and machine learning give you additional confidence in the probability of success in your decision making and accelerate your research and development activities.”
Digital biological twins
Another novel approach being used by scientists at GSK is the use of ‘digital biological twins’ to gain insight into an individual patients’ biology. This is being used across several therapeutic areas at the company.
In oncology, scientists can now build personalised tumour-derived organ-like structures, called organoids, in the laboratory. These can be used to test different treatment combinations in order to ascertain the multi-modal changes (comprised of detailed genomic, proteomic, immunomic and imaging features) in response to the therapeutics tested on them.
The idea is that the success or failure of a particular drug combination in the organoid, combined with the multi-modal characterisation, would predict how well they work in individual patients. This concept is currently being explored in a partnership between GSK and King’s College London.
“We can’t test all the different possible combinations of drugs on a single patient, but we can do it on the organoid because these are renewable resources,” says Professor Tony Ng, SVP of Oncology Translational Research at GSK and cancer research and imaging expert at King’s College London.
“And we can do one-to-one prediction, which ultimately is the personalisation we all need.”
Digital biological twins have the potential to provide even more granular predictions than conventional biomarkers, he adds, telling patients not just which broad category they fall into, but which treatments would work best for their individual cancer based on a symphony of biological information.
“We don't need to say, ‘You fall into that 10% bucket.’ As a clinician, you would like to tell the patient with more accuracy that this is what I think we should do based on the unique characteristics of your tumour.”
Ultimately, GSK’s approach to oncology development is anchored on the promise of finding the right medicine, for the right patient at the right time.
“Oncology is one of those areas where you can work out which patients are the most likely to respond to precision medicines based on biomarker science, and you’re increasing your chances of success,” Sheldon concludes.
“If you can crack it, you’ve got the opportunity for growth and patient benefit. And if you’re having huge growth, it’s because you’re having an impact.”